Dr SSM's Low FODMAP Diet
Low FODMAP diet - introduction

Starting the Low FODMAP Diet
FODMAP stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides And Polyols. I don't know about you, but that sounded daunting when I was studying my six-month accredited course with Monash University on FODMAPs and the Low FODMAP diet. The course was incredibly educational and kick-started my deeper interest in nutrition. Not only did I begin writing more about nutrition, it also changed my own life.
FODMAPs are short-chain carbohydrates (sugars) that are not absorbed directly in the small intestine and instead are fermented by the gut microbes. These FODMAPs are present in many foods such as fruits, vegetables, lentils, nuts, breads, pasta and more. The fermentation process can trigger symptoms in people with IBS or other digestive sensitivities.
Gut bacteria ferment these undigested carbohydrates, producing gases and attracting water into the gut. This can contribute to symptoms such as reflux, bloating, belching, flatulence, constipation, cramps or diarrhoea.
The Low FODMAP diet focuses on the elimination of 6 types of fermentable carbohydrates, including:
-
Fructose — a monosaccharide (made of one molecule of sugar) that can attract water into the gut, especially in those with reduced absorption (especially in people with IBS).
-
Lactose — a disaccharide that requires the enzyme lactase to break it down, which many people lack therefore triggering symptoms.
-
Polyols (sorbitol, mannitol) — they are both small in size like fructose. These sugars are also used as artificial sweeteners and are poorly absorbed therefore ferment and cause symptoms.
-
Oligosaccharides (such as fructans and galacto-oligosaccharides) — these are longer chain carbohydrates that humans cannot digest due to lack of enzymes to break them down.
Starting the Low FODMAP Diet
If you have been prescribed the Low FODMAP diet, it may seem difficult at first. However, this plan is typically short-term and part of a structured elimination process. A strict elimination phase is followed by a careful reintroduction of specific high-FODMAP foods, starting with small amounts and gradually increasing. In most cases, the initial phase lasts about 6–8 weeks before foods are reintroduced one at a time to assess individual tolerance.
Tracking how your symptoms change during reintroduction can help you understand which foods you tolerate or don't tolerate, and this can provide clarity and confidence moving forward.
This is a brief guide intended to help you get started with the Low FODMAP diet. Many people give up early because they are unsure how to follow the plan or lack guidance. My aim is to simplify the concept for you and support you through the initial phase. There are many in-depth resources available, including the Monash University website, books and apps such as the Monash FODMAP app, which I particularly recommend for ongoing guidance.
My Personal Tips for Starting the Low FODMAP Diet
If you're thinking about starting the Low FODMAP diet, here are some gentle suggestions that may make the process easier:
-
Learn the Basics First — Understanding the three main phases (elimination, reintroduction and personalisation) and the overall concept can make the whole journey feel less overwhelming.
-
Download a FODMAP App — Many people find the Monash University app helpful for checking foods and serving sizes when shopping or cooking.
-
Get Support If You Need It — If you're unsure about any part of the diet, check in with your doctor or dietitian for guidance. Everyone's situation is different, and support can make a big difference.
-
Use a Food Diary — Keeping a diary for a week can help you see patterns and plan how to adjust meals more easily during the elimination phase.
-
Plan Your First Grocery Shop — Shopping with a list of low-FODMAP foods can make the first week much smoother.
-
Pair Up If You Can — Doing the plan with someone else (especially if they also have IBS) can make it feel more manageable and even enjoyable.
-
Expect an Adjustment Period — The first week or two can be a little challenging while your gut adapts. Some people notice changes in bowel habits during this phase — this can settle as things adjust.
-
Keep the First Phase Structured — Many people find that keeping high-FODMAP foods out completely during the initial elimination phase helps them assess symptoms more clearly later during reintroduction.
-
Give It a Try — It's only a short-term plan, and for many people it can offer insight into which foods trigger symptoms and which are better tolerated.
The Three Main Phases of the Low FODMAP Diet

1. First step - Avoid
Avoid any high FODMAPs. Low FODMAP diet followed for 2-6 weeks.

2. Second step - Re challenge
Re-introduce the high FODMAP foods slowly. It is best to re-introduce one FODMAP at a time.

3. Third step - Maintanance
Continue with high FODMAP foods which are tolerated. Avoid those which are not tolerated and re challenge at a later stage.
Low FODMAP diet - understanding the principles.
The Low FODMAP diet is primarily a tool to manage symptoms of digestive disorders such as Irritable Bowel Syndrome (IBS). It may be used alongside medical therapy or as a dietary management strategy alone, depending on guidance from your clinician.
FODMAPs are found in a wide range of foods and additives, and are all short-chain carbohydrates that can lead to fermentation in the gut, producing gas and drawing water into the bowel — which can trigger digestive symptoms.
Some people worry that the diet is too restrictive, but using a comprehensive food list or app can reveal that many foods are low-FODMAP or can be consumed in carefully controlled portions.
Nutritional Considerations
A Low FODMAP diet can be nutritionally balanced, but because some high-FODMAP foods are nutritious (e.g., certain fruits and whole grains), careful planning is recommended. Working with a healthcare provider or dietitian can help ensure your diet remains varied and nutritionally adequate.
In individuals with additional conditions such as diabetes, cardiovascular disease, high blood pressure, or chronic kidney disease, the diet may require closer clinical supervision.
Weight and Microbiome
While some people may lose weight during the Low FODMAP diet, weight loss is not its purpose and should not be the reason for following this plan. If weight management is a primary goal for you, you may find the Weight Loss: Unveiling the Hurdles section more relevant.
The Low FODMAP diet can be thought of as a "reboot" of your gut to help manage IBS symptoms, but it is not intended as a long-term elimination diet. Furthermore, as this is a restrictive diet, this will impact the microbiome. A healthy microbiome needs a more plant diverse diet.
Food Guides
The Monash FODMAP app offers a comprehensive and up-to-date list of foods and serving sizes that can help you gauge what is tolerable. Many published books and online resources also provide recipes using low-FODMAP foods. If you download the Monash University app, you will be able to see that some foods with FODMAPs can be consumed in very minimal quantities and should not trigger symptoms.
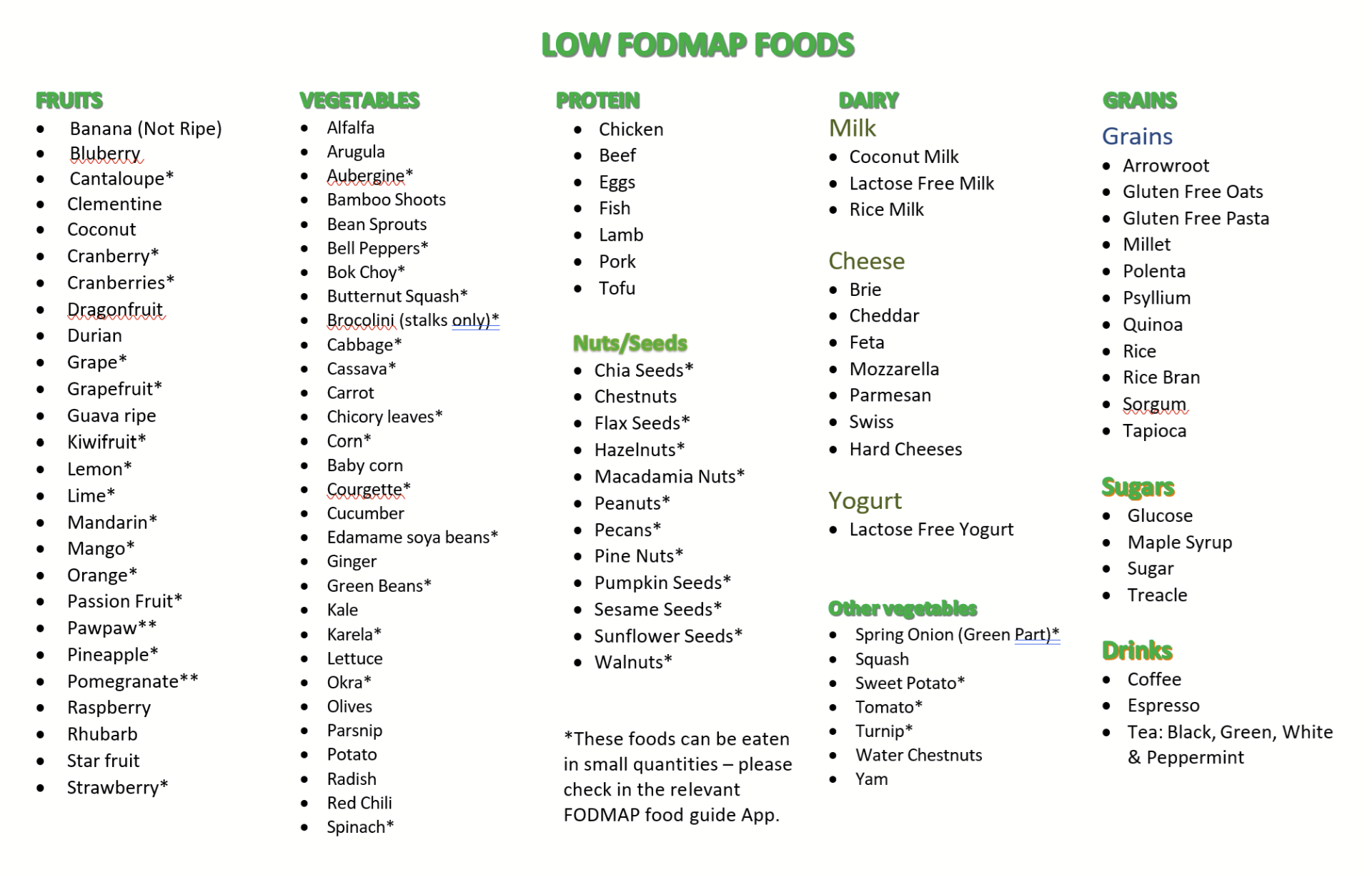
As an addition to my practical tips, I have compiled the list of low FODMAP foods. The starred items in the food list must only be consumed in very small quantities because the FODMAP dose in that portion size should theoretically not trigger symptoms. To see exact amount, the Monash app is the most complete. It is recommended that those with severe symptoms avoid all FODMAPs in the first 2 weeks. The food guides or an app is essential to help you make the correct choices in the initial phase. The best way to start this plan could be to do food diaries and then refer to the food lists from this guide, identify the high FODMAP foods and then replace them with better choices from the low FODMAP list. There are various published books which are easily available on the market, which can help you make recipes using the low FODMAP foods. You can also check my linked recipe section for ideas.

The Three Main Phases of the Low FODMAP Diet - a detailed explanation
1. Restriction — Avoid High-FODMAP Foods
In the first phase of the Low FODMAP diet, all high-FODMAP foods are restricted so that your gut has a chance to settle. The recommended duration may vary, but typically this elimination phase lasts 2–6 weeks, and in some cases up to 8 weeks.
During this phase, meal planning and food diaries can be very helpful. Tracking what you eat and how you feel allows you to replace high-FODMAP ingredients with low-FODMAP alternatives and helps identify personal triggers.
2. Re-introduction — Test Tolerance to High-FODMAP Foods
If symptoms improve during the elimination phase, the next step is to reintroduce higher-FODMAP foods one at a time. This helps determine which specific FODMAPs trigger symptoms and which ones you may tolerate. Always increase the quantity slowly and in small doses before moving on to larger portions.
If symptoms occur after a food challenge, you might choose to avoid that food for now and try re-challenging it at a later stage.
3. Adaptation — Personalise Your Diet
Once you've identified which high-FODMAP foods affect your symptoms, the Low FODMAP diet allows you to personalise your eating pattern. You can continue to include foods you tolerate and avoid those that trigger symptoms. Sensitivity can change over time, and it may be worth re-testing foods that previously caused symptoms.

1. Restriction - AVOID HIGH FODMAP FOODS
Stage 1 of -All foods containing high FODMAPs need to be restricted otherwise the plan is less likely to work.
The time recommended may depend on the Consultant or dietician whom you have seen, and may also depend on your individual case.
Always follow the recommendations made by your doctor or dietician.
The first stage of the low FODMAP diet should typically last for 2-6 weeks or even up to 8 weeks.
You may choose to stop the diet if you see no improvement in symptoms but I would recommend persisting for at least 6 weeks.
I would recommend making food diaries to see which high FODMAP ingredients you can replace with low FODMAP ingredients, therefore planning is the key to success in the first stage.
Utilising the Monash app is highly recommended.

2. Re-introduction - TEST TOLERANCE TO HIGH FODMAP FOODS
Following the initial restriction phase of high FODMAP foods, if symptoms have improved on a low FODMAP diet, then you need to re-introduce some higher FODMAPs back in your diet. This is also important so that you do not develop any nutritional deficiencies.
The re introduction allows you to determine which high FODMAPs were actually triggering your symptoms and which ones you tolerate.
Always re introduce one FODMAP at a time and in small doses first and then slowly build up on the quantity.
If you experience symptoms after a food challenge, you should avoid this food completely, but you can try rechallenging at a later date.
If you do not get any symptoms after a food
challenge, you can assume that the FODMAP is well tolerated and include it as
part of your diet.

3. Adaption - CONTINUE HIGH FODMAP FOODS ONLY IF TOLERANT
You will be avoiding high FODMAP foods that trigger your symptoms and including high FODMAP foods that don't.
If your symptoms return, it could be because you have included a number of high FODMAPs within one meal.
It is also important to remember that sensitivity to high FODMAPs may change over time and therefore it is worth trying to reintroduce any 'failed' high FODMAPs again at a later date.
Avoiding all FODMAPs on a long term is not the recommended solution as it will result in nutritional deficiencies.
Some examples of low and high FODMAPs
The following table shows some examples of low and high FODMAPs in each food category. Full lists of foods can be found in popular FODMAP apps.
Many people may feel put off by how restricted it is. For this reason, it is important to have your FODMAP guide app on your phone because high FODMAP foods in small quantities will not or should not trouble you. These apps will give the exact quantity of the FODMAP you can consume safely per meal.
Although I mention some gluten free options like gluten free pasta, I would recommend to keep the diet as clean as possible by minimising ultraprocessed foods. A lot of gluten free options are extremely ultra processed and not good for our microbiome.
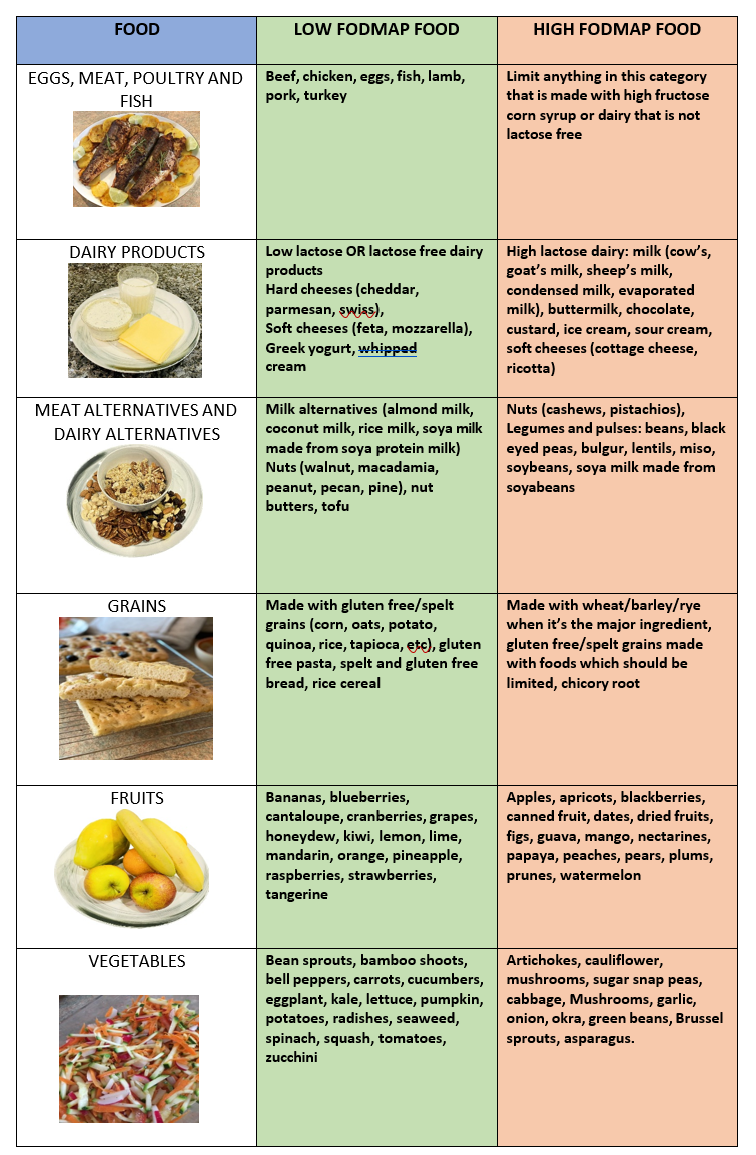
Table showing examples of low and high FODMAP foods. Images are all subject to copyright.
Example of a food diary
The following table illustrates a food diary of a mixture of low and high FODMAPs that a person may have. I have given examples of how the high FODMAPs could be replaced by low FODMAPs. See other ideas see "a day on low FODMAP diet". If anyone loves their bread, once in the re introduction phase, I would recommend trying sourdough instead of the highly processed gluten free breads.
Table showing how to replace food choices in a high FODMAP meal with low FODMAP food choices.
Closing Notes
The Low FODMAP diet is a structured elimination protocol designed to help you find individual food triggers and manage digestive symptoms, particularly in IBS. It should only be used as part of an agreed plan with your healthcare provider or dietitian.
Always speak with your own qualified healthcare professional before implementing this plan. This guide is for educational purposes and is not intended to replace personalised medical advice.
Low FODMAP — Frequently Asked Questions
What conditions is the Low FODMAP diet used for?
Primarily Irritable Bowel Syndrome (IBS), and in some cases digestive sensitivities such as functional bloating, post-infectious IBS, or symptoms triggered after certain foods. It is not a general "healthy diet" or weight-loss diet.
How long do I follow the Low FODMAP diet for?
The strict phase is typically 2–6 weeks (up to 8 weeks). After that, foods are reintroduced gradually to identify which are tolerated. It is not intended as a long-term elimination diet.
Do I need to cut out all high-FODMAP foods forever?
No. The goal is to learn which types and how much you can tolerate, not to avoid them indefinitely.
Can everyone with IBS benefit from this diet?
Not always. Many people do find symptom relief, but responses are individual and may also depend on stress, gut motility, microbiome changes and other factors.
Is this diet suitable for children?
Only under professional supervision. Children have additional nutritional considerations, so guidance from a clinician/dietitian is recommended.
Who should help me follow this diet?
Ideally a dietitian trained in Low FODMAP or a clinician familiar with IBS. Apps such as the Monash FODMAP app can assist between appointments.
Can I do Low FODMAP if I also have diabetes, high cholesterol or high blood pressure?
In many cases yes, but the plan may need modifying. People with chronic conditions should seek individual medical advice before making changes.
What about the microbiome? Does Low FODMAP damage it?
Low FODMAP is short-term, so long-term adverse microbiome effects are unlikely. However, restricting fermentable fibres long-term may reduce beneficial microbial diversity — which is why the reintroduction phase is essential.
Will I lose weight on the Low FODMAP diet?
Some people do, but weight loss is not its purpose. If weight is your concern, other sections (e.g., metabolic health, insulin, microbiome) may be more relevant.
What do I eat if everything seems restricted?
At first it feels restrictive, but many foods are Low FODMAP, and others can be eaten in certain portion sizes. Planning and learning the food lists make it much easier.
Is there an app to help me?
Yes — the Monash University FODMAP App is the gold standard and offers food guides, serving sizes and updates.
Can I reintroduce foods later?
Yes — and you should. Timing varies, but foods are reintroduced gradually after symptoms improve.
What if I feel worse during reintroduction?
It can happen when reintroducing specific foods. It may help to pause, reduce, or try that food later. Sensitivities can change over time.
Is Low FODMAP the same as gluten-free?
No. Some gluten-containing foods (like sourdough wheat bread) can be Low FODMAP in specific portions, and some gluten-free products may be high-FODMAP.
Is this diet safe long-term?
The strict phase is not intended long-term. The personalized phase (phase 3) can be long-term if nutritionally balanced.
Will this cure IBS?
Low FODMAP is a symptom-management strategy, not a cure. IBS has multiple contributing factors including diet, microbiome, gut sensitivity, stress, and motility. Some people find lasting relief; others use it intermittently.
📚 LOW FODMAP DIET — REFERENCES & EVIDENCE
The Low FODMAP Diet Guide (6th edition)
Monash University Department of Gastroenterology.
A practical patient guide explaining IBS, FODMAP categories, the three phases of the diet, portion sizes and meal planning.
Monash University Publishing.
The Monash University Low FODMAP Cookbook (2023)
The Monash FODMAP Team.
Recipe book based on the Monash food testing database, designed for implementation of the diet in real-life settings.
ISBN-13: 9781922633309
Monash University Publishing.
📱 DIGITAL TOOLS (Official App)
Monash University Low FODMAP Diet App
Monash University FODMAP [Mobile Application]
The globally recognised app used to check FODMAP content and portion sizes of foods, based on laboratory testing and ongoing updates by the original research group.
Available on iOS & Android.
Monash University, Department of Gastroenterology.
🧾 ACADEMIC EVIDENCE (Key Scientific Sources)
Evidence for Efficacy & Clinical Use
-
Barrett, J. S. (2017). How to institute the low-FODMAP diet. Journal of Gastroenterology & Hepatology.
Describes practical implementation and symptomatic benefit in IBS.
Mechanisms & Microbiome Effects
-
Staudacher, H. M., & Whelan, K. (2017). The low FODMAP diet: Recent advances in understanding its mechanisms and microbiome effects.
Explores interaction between fermentation, SCFAs, motility and symptom control.
Clinical Review & Evidence Summary
-
Bellini, M., et al. (2020). Low FODMAP Diet: Evidence, doubts and hopes. Journal of Clinical Gastroenterology.
Systematic overview of evidence base, limitations and knowledge gaps.
IBS Management
-
Whelan, K., et al. (2018). The low FODMAP diet in the management of irritable bowel syndrome.
Explains use of the diet in clinical practice settings.
📝 NOTES FOR READERS
• The Low FODMAP diet was developed by Monash University for the management of Irritable Bowel Syndrome (IBS).
• It is a three-phase dietary protocol (elimination → reintroduction → personalisation).
• It is intended to be short-term, with long-term restriction not generally advised without professional supervision.
• Best outcomes occur when supported by a dietitian, clinician or structured guide.

