Microbiome & Gut health
Understanding Gut Dysbiosis: The Link Between Microbiome and Disease
An imbalance in the community of microbes living in our gut is known as microbiome dysbiosis.
This disruption happens when external factors such as poor dietry habits cause the "good" bacteria to decline or lose their diversity. Let's explore how dysbiosis impacts our body...
How Dysbiosis Affects the Body
The microbiome is the front line, like an army, contributing to the strength of our immune system by creating a protective lining in our gut, protecting us from harmful chemicals and pathogens. They make postbiotics like Short-Chain Fatty Acids (SCFAs) that help strengthen the protective mucus layer. Not only do they protect us from chemicals and pathogens, the bacteria also help regulate our response to foods. They can help reduce glucose spikes and how our fat levels rise in the blood.
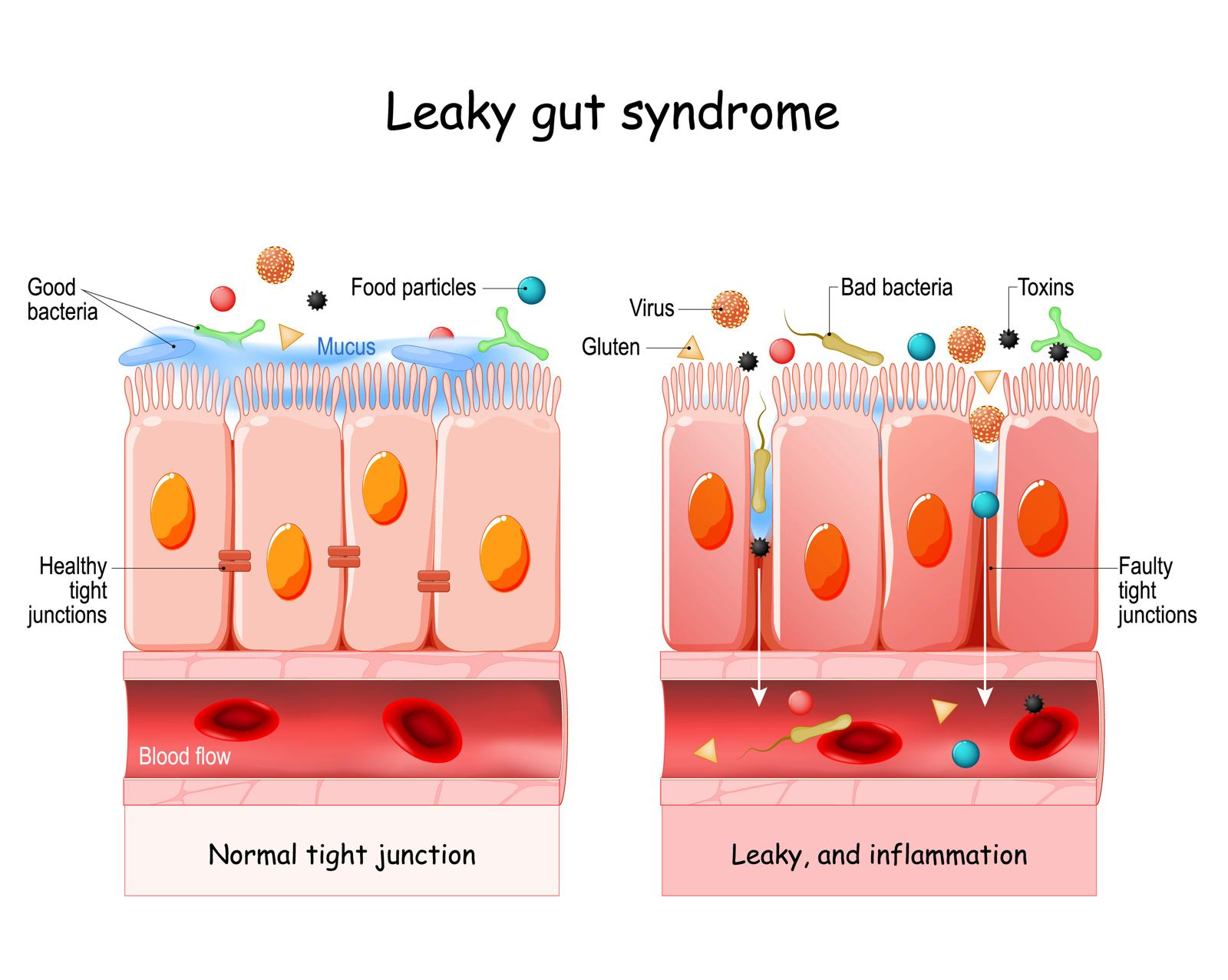
When our gut bacteria are out of balance, they produce fewer SCFAs like butyrate. Without them, the lining weakens, leading to what is often called a "leaky gut", also known as leaky gut syndrome. Usually the gut cells are tightly packed together, protected from the mucus layer and good bacteria, allowing the bacteria to make chemicals for vital physiological and biochemical processes. In a leaky gut, the mucus layer gets disrupted and the cells develp gaps.
The leaky gut allows toxins and pathogens to "leak" into the bloodstream, triggering an immune response and many other inflammatory processes. This doesn't just stay in the gut; it can cause a full-body inflammatory response, leading to:
Short-term symptoms: Fatigue, poor sleep, low mood, joint pain, and skin issues.
Long-term chronic diseases: Obesity, Type 2 diabetes, heart disease, metabolic syndrome, and non-alcoholic fatty liver disease.
Systemic issues: Links to autoimmune diseases and neurodegenerative conditions.
The microbiome is not just for digestion...
The microbiome balance in the gut is important for many important physiological functions:
- Keeping the gut lining intact and maintaining good immune function
- Many neurotransmitters are formed here which are important for our brain health and the gut-brain axis
- Food digestion happens here ensuring delivery of our nutrients (for example break down proteins in to amino acids), vitamins (such as vitamin K), and minerals (such as magnesium, calcium and iron) necessary for cellular function in the whole body
- a symbiosis at the gut level results in less over inflammation in the body
- the gut microbiome helps regulate our metabolic responses including glucose spike, insulin levels and other hormones
Pathogens and chemicals include viruses, bacteria, additive in foods, sweeteners, emulsifiers and even medications.
High glucose consumption also weakens the gut lining.
What Causes Gut Dysbiosis? (Common Disruptors)
Microbiome disruption is rarely random. The biggest triggers include:
• Poor diet high in sugar & ultra-processed foods
starves beneficial microbes and feeds inflammatory species.
• Antibiotics & other medications
broad-spectrum antibiotics reduce microbial diversity for months; PPIs increase SIBO risk; NSAIDs increase gut permeability.
• Artificial sweeteners & food additives
emulsifiers, stabilisers and certain sweeteners can impair the mucus barrier and alter glucose responses.
• Pesticides & environmental chemicals
residue can negatively impact beneficial strains and metabolic pathways.
• Chronic stress & poor sleep
disrupt the gut-brain axis and change motility, hormones & microbial balance.
• Low fibre intake
reduces SCFA production (like butyrate) needed for gut barrier protection.
• Sedentary lifestyle and irregular eating habits
linked to decreased microbial diversity and slower gut transit.
• Recurrent infections or inflammation
can wipe out protective species and allow pathogenic overgrowth.
The more triggers present, the harder it becomes for the microbiome to maintain balance — moving from symbiosis to dysbiosis.
Enivronmental & other factors:
• Smoking & alcohol can alter microbial balance and increase gut inflammation.
• Environmental toxins, pesticides and pollutants may affect microbial ecosystems.
• Age, genetics and chronic illness also influence microbial composition and resilience
Longer fasting windows activate the migrating motor complex (MMC), the gut's natural 'clean-up wave', which helps prevent bacterial overgrowth in the small intestine.
Falling oestrogen during perimenopause/menopause reduces microbial diversity, alters bile acid metabolism and worsening metabolic flexibility, mood, gut motility and fat distribution.
A Holistic Shift in Medicine
Understanding the microbiome is a game-changer for modern medicine because it puts power back into the hands of the patient. While everyone's microbiome is unique—meaning there is no "one-size-fits-all" cure—lifestyle modifications can make a massive difference.
Research into conditions like Inflammatory Bowel Disease (IBD) shows a clear difference between the gut bacteria of healthy individuals and those with the disease. While we are still learning whether the dysbiosis causes the disease or the disease causes the dysbiosis, it is clear that the two are deeply interconnected.
The Role of Insulin Resistance
Microbiome dysbiosis is also closely linked to insulin resistance, a major driver of modern health problems like pre diabetes, diabetes, Non-alcoholic Fatty Liver Disease, high cholesterol, obesity, cardiovascular disease and various other metabolic diseases. Improving your gut health is one of the most effective ways to manage how your body processes the macronutrients such as carbohydrates and fats.
How Dysbiosis Leads to Insulin Resistance
When the gut microbiome becomes imbalanced (dysbiosis), the protective mucus layer and tight junctions of the gut lining can weaken. This allows fragments of bacterial cell walls — particularly lipopolysaccharides (LPS) from gram-negative bacteria — to pass into the bloodstream. This process is known as metabolic endotoxemia.
Once in the bloodstream, LPS acts as a low-grade inflammatory trigger by activating the immune system. Over time, this persistent inflammation interferes with insulin signalling in liver, muscle and fat cells. This is a key mechanism behind insulin resistance, a condition where the body needs more and more insulin to control blood sugar.
Insulin resistance sits at the root of many modern health problems including:
-
pre-diabetes and type 2 diabetes
-
non-alcoholic fatty liver disease (NAFLD)
-
metabolic syndrome
-
obesity (especially central obesity)
-
high cholesterol and raised triglycerides
-
menopausal weight gain
-
cardiovascular disease
A healthier microbiome supports insulin sensitivity by:
-
producing short-chain fatty acids (SCFAs) like butyrate
-
strengthening the gut barrier
-
reducing inflammation
-
improving glucose regulation and satiety signalling
Dysbiosis → Leaky Gut → LPS → Insulin Resistance → Metabolic Syndrome
How to "Fix" Your Microbiome
Fix Microbiome & Fix Gut Health
The good news is that you can improve your gut health by changing your environment and diet. It isn't just about what you eat, but how you eat.
Dietary Changes
Eliminate Ultra-Processed Foods: Avoid additives like emulsifiers, stabilizers, and artificial colorings.
Cut the Sugar: Reduce refined sugars and avoid artificial sweeteners.
Ditch Refined Oils: Stop using "bad" refined seed oils.
Focus on Diversity: Aim for 30 different plants per week to increase bacterial diversity.
Eat Real Food: Choose whole grains over processed flours and opt for organic where possible to minimize pesticides.
Prebiotics & Probiotics: Incorporate natural sources of both (like onions, garlic, kimchi, and kefir) rather than relying solely on supplements.
I go in to a lot more depth in how to clean up the diet. Explore more on how to clean up the diet.
Lifestyle Habits
Manage Stress: Chronic stress physically alters your gut environment.
Prioritize Sleep: Poor sleep and poor gut health exist in a vicious cycle.
Change Your Timing: Minimize snacking and increase the time between meals.
Intermittent Fasting: Aim for a minimum of 12 hours between dinner and breakfast to give your gut time to repair itself.
Exercise. Stay physically active and maintain regular meal times.
Other tips
-
Avoid unnecessary acid-suppressing medications when possible (discuss with clinician).
Use antibiotics only when necessary and complete prescribed courses under guidance.
Why These Changes Matter
The gut microbiome does more than help digest food:
- supports immune system regulation
- produces beneficial metabolites like butyrate
- communicates with the brain (the gut–brain axis)
- influences metabolism, inflammation and hormone balance
When the microbiome is damaged, these functions are impaired, increasing the risk of inflammatory processes, metabolic disorders and digestive symptoms.
